Shin Pain and it's Cure
Kill Shin Splints
Shin refers to the bone located on the front of the lower leg (i.e. below the knee). Extra pressure on the lower extremity may result in muscle strain which is considered to be a common cause of swelling and tenderness below the knee. The most common cause of shin pain is trauma or injury to the feet. Though little bit of rest and cold compression is the trick, on some occasions shin pain is chronic in nature and requires a long term treatment therapy. Simple home remedies are beneficial in the management of shin pain. Shin splints is a nonspecific term typically used to describe exertional leg pain. Although common in runners, this condition probably is overdiagnosed. The connective sheath attached to the muscles and bone of the lower leg become irritated, resulting in a razor-sharp pain in the lower leg along the inside of the tibia or shin bone. Pain can be felt anywhere from just below the knee down to the ankle. It usually develops after physical activity, such as vigorous exercise or sports. Repetitive activity leads to inflammation of the muscles, tendons, and periosteum (thin layer of tissue covering a bone) of the tibia, causing pain. The bone tissue itself is also involved. The condition is also referred as
• Medial Tibial Stress Syndrome (MTSS)
• Medial Tibial Traction Periostitis
• Medial Tibial Periostitis
Relevant Anatomy
The leg bones (tibia and fibula) serve as the origin for the extrinsic muscles of the foot and ankle. The muscles of the leg are surrounded and divided by the crural fascia. The resulting compartments (anterior, lateral, superficial, posterior and deep posterior) are unyielding with regard to volume and are prone to develop increased pressure. The anterior compartment contains the extensor muscles, including the anterior tibial, the extensor digitorum longus, and the extensor hallucis longus muscles. The posterior medial tibia serves as the origin for the posterior tibial muscle, the flexor digitorum longus muscle, the soleus muscle, and the deep crural fascia.Etiology
There are a number of different causes of shin splints. The main causes are listed below.
Stress fractures - These are an overuse injury. They develop after repeated periods of stress on your bones; for example, running or dancing over a long period of time.
Medial tibial stress syndrome - This is inflammation where the tendon attaches to the thin layer of tissue that covers the bone (periosteum). Medial Tibial Stress Syndrome has been reported to occur frequently in military recruits, distance runners, dancers, football (soccer) players and gymnasts. Medial Tibial Stress Syndrome has been classified into two distinct types, which affect specific tissues on the inside of the shin:
• Type One
This is characterised by a stress reaction on the inside border of the shin bone. A stress reaction is a preceding stage to a stress fracture.
• Type Two
This is characterised by irritation of the outer surface (periosteum) of the inside of the shin bone at the point where the Soleus and Tibialis Posterior muscles attach.
Regardless of the type, Medial Tibial Stress Syndrome is largely caused by over-use, with those who run regularly on hard or uneven surfaces being particularly affected. However, there are a number of factors, such as altered foot, knee and hip posture, which can make a person susceptible to the syndrome.
Compartment syndrome - This happens when your muscle swells. Your muscle is confined by the compartment it's in, so doesn't have much room to expand. When the pressure in your muscle increases it causes the symptoms of compartment syndrome.
 |
| Compartments of leg |
Anterior shin splint are related to dysfunction of the anterior leg compartment or its contiguous structures. Medial tibial stress syndrome is the clinical entity that most likely represents medial shin splints. The exercise induced pain associated with medial tibial stress syndrome tends to involve the distal two thirds of the leg. The etiology of anterior shin splints is not completely understood; overuse or chronic injury of the anterior compartment muscles, fascia, and bony and periosteal attachments is most commonly implicated. The most common cause of medial tibial stress syndrome is a traction periostitis of the soleus or flexor digitorum longus muscle origins.
Possible causes include:
• Flatfeet (pronated) or abnormally rigid arches.
• A sudden increase in running speed.
• A sudden change from soft to hard running surfaces.
• Running in worn down shoes.
• Tight Achilles and calf muscles.
• An inexperienced runner just beginning to run.
• Running on uneven terrain.
• Excessive uphill running.
• Poor running mechanics which include excessive forward lean, excessive weight on the ball of the foot, running with toes pointed outward, landing too far back on the heels causing the foot to flap down, and overpronation.
Symptoms
It cause pain in the front of the outer leg below the knee. The pain is characteristically located on the outer edge of the mid region of the leg next to the shin bone (tibia). An area of discomfort measuring 4-6 inches (10-15 cm) in length is frequently present. Pain is often noted at the early portion of the workout, then lessens only to reappear near the end of the training session. Shin splint discomfort is often described as dull at first. However, with continuing trauma, the pain can become so extreme as to cause the athlete to stop workouts altogether.Diagnosis
A diagnosis of shin splints is suggested by a history of exercise induced pain at the distal two thirds of the leg. The pain is localized to the anterior compartment in anterior shin splints and to the distal two thirds of the posterior medial tibial border in medial tibial stress syndrome. There is exercise induced leg pain which is relieved by decreased activity. The condition is never associated with vascular or neurologic symptoms or findings.On examination, patients with medial tibial stress syndrome will often be tender over this same part of the tibia. Patients may or may not have a small amount of detectible swelling over this part of the tibia. Some specific maneuvers, especially resisted plantar flexion (pushing down of the foot against resistance), typically causes an increase of symptoms.
In order to determine the underlying cause of the MTSS your physician may order an x-ray or a bone scan. The x-ray can detect fractures, and occasionally detect long-standing stress fractures. The bone scan will detect areas of high bone turnover; these ‘hot’ areas indicate possible stress fractures or other bone problems. Early and correct diagnosis helps in prompt shin splints treatment.
Differential Diagnosis
• Fibular stress fracture- Exertional pain at fibula; pronation or valgus alignment; point-tender fibula; abnormal radiograph, bone scan, CT or MRI.
• Acute compartment syndrome- Leg pain secondary to trauma, tender compartments, pain with passive movements, decreased sensations, elevated compartment pressure, paresthesias.
• Chronic exertional compartment syndrome- Exertional leg pain, no acute trauma, tender compartments, decreased sensation after exertion, elevated post exertion compartment pressures, paresthesias.
• Congenital anomaly- Exertional leg pain, no acute trauma, anomalous muscle such as accessory soleus, symptoms similar to chronic exertional compartment syndrome, accessory muscle identified on MRI.
• Tumor- Night pain, abnormal radiograph, bone scan, CT or MRI.
Shin Splints Treatment
Acute exertional pain associated with MTSS is treated with RICE regimen until symptoms subside. Increasing rest intervals and duration are also beneficial to both types of shin splints. Running is prohibited until the patient is pain free.
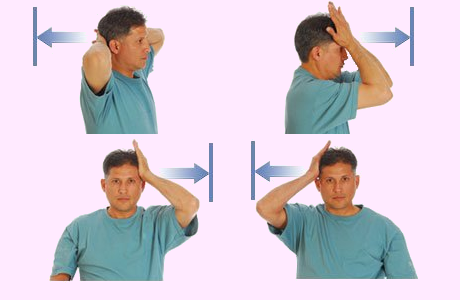
The protocol for a sports person involves rest and ice, strengthening and stretching exercises, followed by a gradual return to running after symptoms subside. In order to help prevent recurrence of the condition, a bio-mechanical analysis (an analysis of posture at rest and during walking and running) with a physiotherapist or podiatrist can be very useful. This will pick up any factors that may be making a person susceptible to Medial Tibial Stress Syndrome, so that they can be corrected before a return to activity.
Muscle imbalance and leg length inequality are frequent causes of mal-alignment that can be picked up during the physiotherapy assessment. A common cause of Medial Tibial Stress Syndrome is pes planus (flat feet) or pronated foot position (a lowered arch during running). These would be identified during bio-mechanical analysis. Over pronation is the uncontrolled lowering of the arch of the foot during running. This puts increased strain on the Tibialis Posterior muscle which pulls on the inside of the shin and can produce pain. Arch supporting Orthotics insoles can be very effective in remedying this problem.
All cases of pain in the shin should be properly assessed by a chartered physiotherapist or anorthopaedic consultant as shin conditions can be made worse by continuing with exercise. The best way of maintaining fitness during this time is to use non weight bearing exercises in the swimming pool. Running without touching the bottom of the pool while wearing a Buoyancy Belt is a great method of maintaining fitness while allowing the injury to heal.
In cases of shin pain that have been investigated by a doctor and found to be a soft tissue problem, many people find that a Compression Sleeve can be an effective treatment that allows them to run. Compression sleeves work by restricting the pull of muscles in the shin, which can reduce the stresses on the shin during running. Without being a cure for Shin Splints, they can effectively reduce symptoms, allowing runners to get round.
Anterior shin splints treatment with aggressive warm up and stretching, with particular attention to the gastrosoleus-Achilles tendon complex. Anterior symptoms may also respond to decreased shoe weight and level running surfaces.
Medial tibial stress syndrome is treated in similar fashion with antipronation taping and orthotics and running on a non banked, firm surface. Stretching and flexibility is emphasized throughout rehabilitation program.
Surgery is never indicated for anterior shin splints treatment. For recalcitrant medial tibial stress syndrome, deep posterior compartment fasciotomy and release of the soleus musle origin off the posterior medial tibial cortex have been suggested.
0-3 Days: Acute stage shin splints treatment
• Relative rest, ice massage and whirlpool.
• Ultrasound therapy if no bony involvement.
• Isometrics.
• Seated towel scrunches -- a towel placed on the floor. The towel crunch exercise calls for resting your foot on a towel, then using your toes to move the towel toward your heel.
• Cycling
• Water activities (deep water running). Hydrotherapy/pooltherapy.
• Gastrocnemius and soleus stretching.
• Massage
Day 4-Week 6: Subacute stage shin splints treatment
This stage begins with resolution of weight bearing pain and ends with resolution of activity related pain.
• Modalities to decrease inflammation are continued.
• Emphasis remains on increasing flexibility.
• Theraband exercises.
• Towel scrunches progressed from seated to standing position.
• Balance training are begun with progression of difficulty.
• Aerobic fitness is maintained with cross training activities such as slideboard, water running and cycling.
Week 7: Return to Sport stage shin splints treatment
• Running started once pain has resolved.
• Warm up and stretching.
• Patients are to initially avoid running on uneven surfaces.
• Attention is first directed to reestablishing distance, followed by speed.
• Antipronation orthotics for patient with MTSS or low dye taping.
.jpg)






.jpg)






.jpg)

.jpg)
Comments
Post a Comment